What is Brain Trauma?
Brain trauma is an acquired injury to the brain that can be caused by either physical trauma (traumatic brain injury) or a psychological experience (post-traumatic stress).
Post-traumatic stress disorder (PTSD) is a clinically diagnosed condition that develops in some people who have experienced a shocking, scary, or dangerous event.1 The associated stress of experiencing or witnessing this trauma can cause physical changes in the brain.
Traumatic brain injury (TBI) is defined as damage to the brain resulting from external mechanical force, such as rapid acceleration or deceleration, impact, blast waves, or penetration by a projectile.2

For both PTSD and TBI, the trauma can lead to changes in the structure and function of the brain that result in a variety of cognitive, physical, and emotional symptoms. Some of these symptoms may appear immediately after the traumatic event or brain injury, while others may be delayed, emerging months or even years later.
PTSD and TBI often coexist, and many of the symptoms of PTSD and TBI overlap. This can make it difficult to attribute the resulting symptoms to one disorder or the other and also can lead to misdiagnoses and delays in treatment. Both PTSD and TBI can greatly impact a patient’s health in terms of increased risk for other conditions such as cardiovascular disease, hypertension, hyperlipidemia, and obesity, as well as a number of psychological disorders such as depression, anxiety and substance use disorders.

Brain Trauma and Suicide
Both PTSD and TBI can increase the risk for suicide. Increased suicide risk is of particular concern among Veterans and service members. Studies by the Department of Veterans Affairs find that a history of TBI or PTSD is associated with a substantially increased likelihood of suicide attempts compared to those without the diagnosis — 1.5 and 2.8, respectively. For those with both TBI and PTSD, the likelihood of a suicide attempt is 3.3 times greater than for those with a TBI alone.
Studies among civilians also show a link between suicide and a history of PTSD and/or TBI.
Trauma can happen to anyone.
Tragically up to 22 American Veterans and service members die by suicide daily.

In a global survey, 70% of respondents reported witnessing or experiencing a traumatic event.

Every 5 seconds, a man, woman or child in the U.S. suffers a traumatic brain injury.
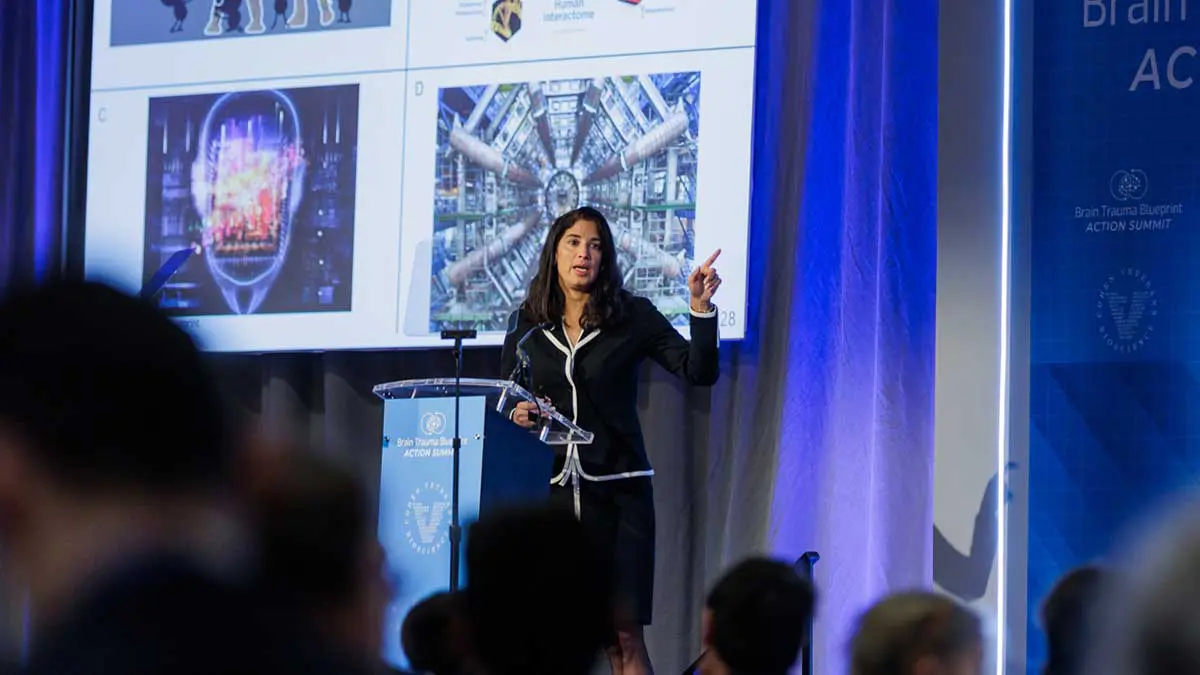
Millions affected by brain trauma are still waiting for solutions
Despite the frequency of brain trauma, decades of promising research and billions spent on clinical studies:
- There are no cures for brain trauma.
- Patients are diagnosed based on subjective, patient-reported symptoms, and not in an objective way based on their unique biology.
- We lack reliable, evidence-based treatments.


Our mission is to fast-track and advance solutions to diagnose and treat PTSD and TBI. No one who experiences brain trauma should have to suffer the effects for a lifetime.
Resources and Further Reading
- If you have taken steps to end your life, call 911 immediately.
- National Suicide Prevention Hotline – Dial 988
- National Sexual Assault Hotline – (800) 656-HOPE
- National Center for PTSD – Veterans Crisis Line – (800) 273-8255
- Women’s Veterans Call Center – (855) VA-Women
Sources / Citations
1 National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd
2 Maas AI, Stocchetti N, Bullock R (August 2008). “Moderate and severe traumatic brain injury in adults”. The Lancet. Neurology. 7 (8): 728–741. doi:10.1016/S1474-4422(08)70164-9. PMID 18635021. S2CID 14071224.