Candy, apple, coin! I repeated these three simple words slowly, clearly and confidently during a brain test at the Office of my wonderful doctor. Jeff, a highly skilled healthcare professional, had given the words to me during the exam as he moved on with other brain tests. He then quizzed my memory.
Remembering three simple words was my Thanksgiving gift on Monday, November 23, 2015. My heart beat joyfully many times during that appointment. As my physician proceeded with his iterative, thorough, neurological tests on me, I could see positive change. My word recall was matched by better balance, as well as on that day, responding negatively to all symptoms on his brain checklist of 20 questions given to concussion patients during every appointment. I had no headaches, no broken sleep, no anxiety or sadness, no disorientation, and no fatigue. When he asked me to follow his index finger in front of my eyes, I could do so without the feeling of a heavy weight on my eyelids – a noticeable improvement.
As a result, he was able to release me from his care after seeing me every two to three weeks since an automobile accident on July 31st. He reassured me that his staff and he were available by phone if I had any questions in the future. I expressed my gratitude to him and his terrific staff in that moment of good news.
As a writer, researcher, and consultant doing work on national policy with the US Congress on brain disease, I rely on my ability to use my words carefully. Over the last three years, I have organized an annual conference on Capitol Hill to gather experts, members and staff of the US House and Senate, and other advocates on challenges to a law that requires our insurers to treat physical and mental benefits equally or in parity.
My doctor told me during my first visit on August 5th that if I listened to his advice, I could expect full recovery. If I did not, I would delay it. Throughout these weeks, I kept that serious advice front and center of my busy life. As a result, I sense now at more than 85 percent recovery that full recovery will come in 2016.
While struggling to work full-time, I was able to learn the tools of managing not only the headaches, balance issues, memory challenges, sleeplessness, and anxiety, but also the main element of the beginning, the fear. I learned to rest and to pace my exposure to my work on the computer, cell phone texts and television. I did limited workouts through daily walks in my neighbor’s backyard pool and around my borough. I convinced myself to sleep longer in the morning and go to bed earlier at night. I took fish oil and melatonin every day and night. I ate salmon regularly. I learned to let go of stress and focus on what mattered most each day.
At the very start, my physicians seriousness of purpose and tone put the fear of God into me about following his words and advice so that eventually he and his staff saw me as the poster child of a well behaved concussion patient. Yet, this prize is not the most cherished; rather it has become my newly acquired knowledge about unseen wounds.
My doctor works with the athletes of the Philadelphia Union, our region’s professional soccer team, and many county public and private school athletes. Concussions are trending upwards among school athletes throughout the nation. These cases serve also as a point of common ground with concussion cases sustained in car accidents as well as from injuries occurring from war.
Some telling statistics about our returning veterans as reported by the American Psychiatric Association include: 300,000 veterans of the wars in Iraq and Afghanistan have been diagnosed with PTSD; more deaths by suicide than by war combat in 2012; 8 to 20 percent of military personnel deployed in Iraq or Afghanistan experienced a traumatic brain injury; 20 percent of national suicides are completed by veterans; military suicide are at their highest rate in ten years; and traumatic brain injuries can increase suicidal thoughts and behavior.
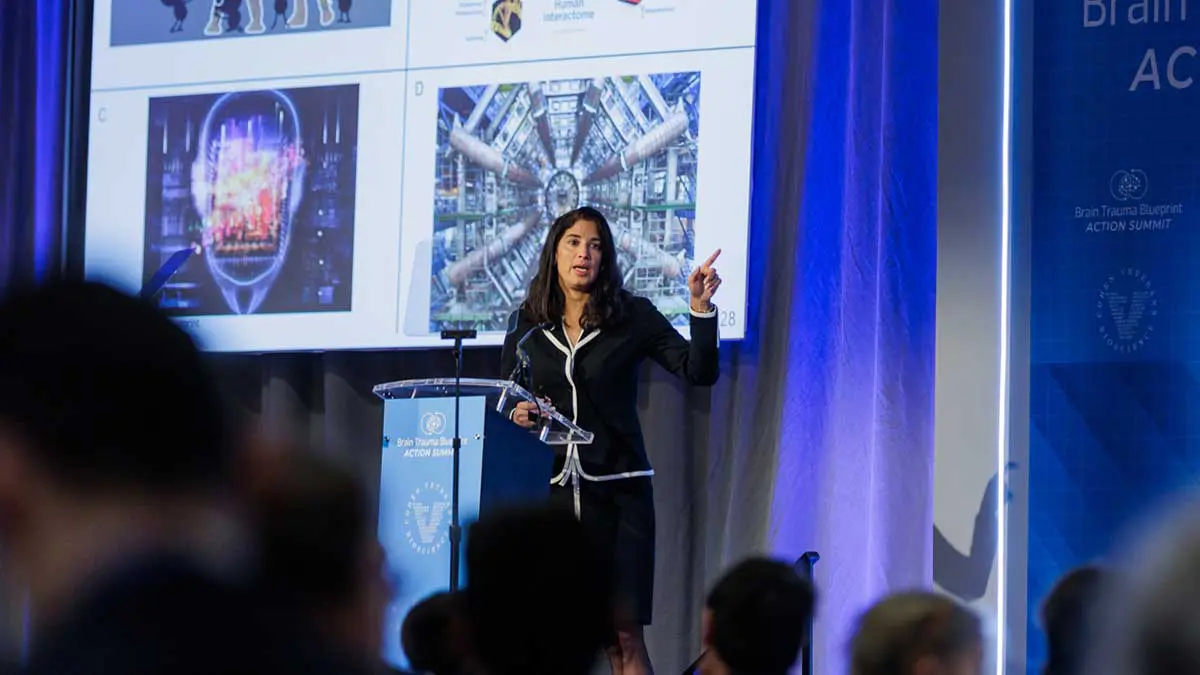
In December 2015, Cohen Veterans Bioscience’s CEO Magali Haas sponsored my third annual roundtable on the Mental Health Parity Addiction and Equity Act of 2008. She co-led a panel with retired US Army Colonel Dallas Hack on the need for a national model to treat the veterans with PTSD and TBI. Cohen Veterans Bioscience is harnessing the power of high-performance computing and data analytics to discover and develop predictive disease models from integrated biomarker, biosensor, and phenotypic data. The hope is that, in the next three years, there will be a first generation of diagnostics for PTS and TBI. “Once we have a better understanding of the science of PTS and TBI, we can advance a new pipeline of therapeutics and improve the delivery of medical care,” says Dr. Haas.
As I said to my physician throughout last year, my personal life has brought me a real lesson of empathy and insight into the challenges of these veterans as well as other patients suffering with concussion, which I can now bring to my professional work. This motivation is more than enough to follow the good doctor’s advice while hoping and working for FULL RECOVERY in 2016.