These brave men and women voluntarily stepped up on the line to serve this great nation with the goal of protecting our freedoms…many have gone into harm’s way at personal expense and sacrifice. We cannot leave any more of them behind. It is our national obligation to support those that have come home with both visible and invisible wounds.
Frank Larkin
Member, Veterans Advisory Council
The VAC’s Goals
- Share Veterans’ perspectives, challenges, and needs to inform research that will help improve the health of Veterans
- Lead awareness efforts to build support for researching brain trauma solutions from within and outside of the Veterans’ community
- Increase collaboration across the community to help prevent, diagnose, and treat PTSD, TBI, and other co-morbid conditions
- Reinforce legislation to advance the execution of a comprehensive plan that accelerates PTSD and TBI research.
- Raise awareness of brain trauma as a risk factor for suicide and drive efforts to address suicide through research.

The VAC’s Advocacy Priorities
- Improving Veterans’ access to high-quality mental health care
- Leveraging large-scale collaborative research roadmapping efforts
- Increasing the body of evidence on emerging therapeutic solutions
- Ensuring full implementation of important mental health legislation
Council Members

Jane Horton
Member, Veterans Advisory Council
Jane Horton
Member, Veterans Advisory Council
Ms. Jane Horton is a respected and influential global leader for national security, humanitarian, and veterans. A fearless and relentless advocate, she successfully fosters bipartisan collaboration on legislation, policies, and programs to better the lives of veterans, service members, their families, and those across the globe. Jane currently serves as a senior policy advisor in the United States Congress in Washington D.C. Previously, Jane was a senior advisor in the Office of the Secretary of Defense in the Pentagon. In this capacity, she advised on civilian and military personnel policy, military family policy, and international security affairs. She championed efforts to advance warfighter brain health and Gold Star family initiatives and has inspired or authored over twenty pieces of legislation in over a decade. Some of Jane’s additional experiences include serving as a special assistant to the Chairman of the Joint Chiefs of Staff, General Joseph Dunford, an advisor to the Chief of Staff of the Army, and the congressional and military liaison to the Ambassador of Afghanistan to the United States. She currently serves on the board of directors of numerous non-profits and is a proud member of Georgetown University's US- Afghan Women's Council.

Robin King
Member, Veterans Advisory Council
Robin King
Member, Veterans Advisory Council
Ms. King has been with the Navy SEAL Foundation since its inception in July 2000, and in that time has served as Chief Financial Officer, Deputy Executive Director, and Interim Executive Director before being appointed as Chief Executive Officer in May of 2013. Her exemplary leadership and commitment to financial transparency and accountability have allowed the Foundation to grow from a small organization focused on scholarships and educational opportunities to a multi-faceted programmatic foundation with dozens of specialized programs and an annual program budget in the millions.
Ms. King executes the daily mission of the Navy SEAL Foundation from Coronado, California, home of Naval Special Warfare Command (WARCOM), SEAL Qualification Training and the headquarters of NSW. She leads a staff of nearly twenty employees located throughout the United States. Under her command, the Navy SEAL Foundation has consistently achieved and maintained the highest rating possible from Charity Navigator, a national charity watchdog organization, placing it in the top 1% of all charities rated.
In August of 2019, Ms. King was awarded the prestigious United States Special Operations Command (USSOCOM) Outstanding Civilian Service Medal which recognized her steadfast dedication and superior service to the NSW community including raising millions of dollars to fund programs touching the lives
of tens of thousands of NSW warriors and families.
In 2017, Ms. King was awarded the USSOCOM Care Coalition Patriot Award. This distinguished award recognizes individuals and organizations who greatly support Special Operations Force (SOF) wounded warriors, their families, and surviving family members by providing significant and enduring
contributions that benefit their care and recovery. She is the first nonprofit leader to receive this award.
Ms. King is a current member of the Board of Directors for The Honor Foundation and the C4 Foundation, both nonprofits serving the Naval Special Warfare community.
Before her employment at the Foundation, Robin worked at Pacific Trust Bank, The Walt Disney Company, and McDonnell Douglas Corporation (Boeing). She holds a Bachelor of Science degree in Business Administration, Finance, from California State University, Long Beach.
Frank Larkin
Member, Veterans Advisory Council
Frank Larkin
Member, Veterans Advisory Council
Frank Larkin was formerly the United States Senate Sergeant at Arms (SAA). As chief law enforcement and executive officer of the Senate, the SAA enforces rules of the Senate; provides a range of technical and administrative services to Senators in their Washington, DC, and state offices; and maintains security in the Capitol and Senate office buildings.
Frank was a member of the Senior Executive Service, recently serving as both the Acting Director and the Vice Director of the Joint Improvised Explosive Device Defeat Organization (JIEDDO) within the Department of Defense. He previously served as JIEDDO’s Director for the Counter IED Operations-Intelligence Integration Center. JIEDDO’s mission was to focus all Department of Defense actions in support of the combatant commanders’ efforts to defeat improvised explosive devices (IEDs) as weapons of strategic influence. Frank’s focus was in support of our deployed warfighters and special operations forces around the globe and the integration of a “whole of government” disruption effort targeting extremist networks that employ IEDs.
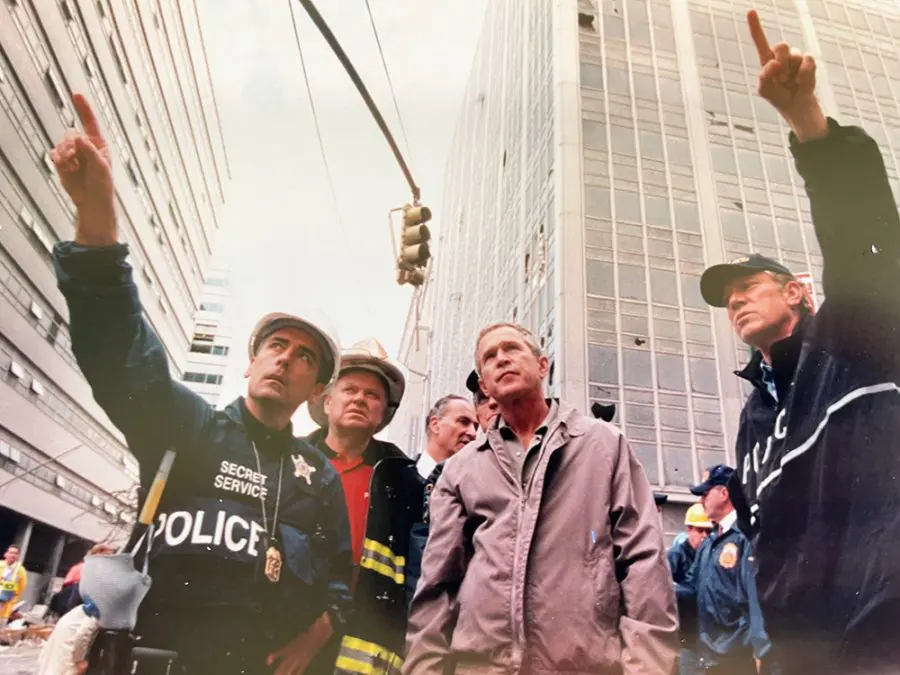
Frank served for more than two decades in the United States Secret Service (USSS), beginning in 1984 as a Special Agent assigned to the Philadelphia and Washington Field Offices, before assignment to the Presidential Protective Division. He was assigned to the Office of Congressional Affairs for a two-year fellowship on Capitol Hill, serving a year each with the Senate and House Appropriations Committees. Frank entered the USSS supervisory ranks as Assistant to the Special Agent in Charge of the New York Field Office, where he led financial, electronic, and organized crimes investigations. Following the events of 9/11, he returned to Washington, DC, as the Assistant Special Agent in Charge of the Presidential Protective Division, supervising White House security operations. As Assistant Special Agent in Charge of the Technical Security Division, Frank was responsible for tactical countermeasures programs. In 2004, he was promoted to the Senior Executive Service, assuming the position of Deputy Assistant Director for Protective Research and Chief Technology Officer.
Following his USSS career, Frank was Director, Program Management & Leadership, for the Raytheon Company, and more recently, worked at Lockheed Martin’s Defense & Intelligence Solutions, responsible for providing operations and intelligence analysis support to the intelligence community.
A veteran of the US Navy, Frank has a significant military and law enforcement special operations background, serving as a special warfare operator in the Navy SEALs. After his Navy service, he was a uniformed patrol officer with the Norristown (PA) Police Department, a homicide detective with the Montgomery County (PA) District Attorney’s Office, and a Maryland State Trooper-Flight Paramedic.
Frank holds a BA degree in criminal justice and an MS degree in public administration from Villanova University. He is the recipient of numerous awards, including the US Secret Service award for valor, the Department of the Army’s Exceptional Civilian Service award, and the Superior Civilian Service award.

LTG John F. Mulholland, U.S. Army (Ret).
Member, Veterans Advisory Council
LTG John F. Mulholland, U.S. Army (Ret).
Member, Veterans Advisory Council
The proud son of a USAF fighter pilot and Korean War veteran, Lieutenant General Mulholland John Francis Mulholland, Jr. (Retired) was born in Clovis, New Mexico, but grew up in Bethesda, Maryland. He earned a Bachelor of Arts in History and was commissioned as a Second Lieutenant of Infantry, United States Army upon graduating from Furman University, Greenville, South Carolina, in 1978.
As a young Infantry officer, LTG Mulholland (Ret) served as platoon leader of both mechanized and airborne rifle platoons, as well as mortar platoon leader. Since joining the 1st Special Forces Regiment in 1983, LTG Mulholland (Ret) commanded from the captain through lieutenant general-level in Army and joint special operations forces, including serving as Deputy Commanding General, Joint Special Operations Command, as the Commanding General, United States Army Special Operations Command, and as the 15th Deputy Commander, United States Special Operations Command. Following graduating from the National War College in 2001, then-COL Mulholland assumed command of the 5th Special Forces Group, Airborne at Ft. Campbell, KY. In the immediate aftermath of the attacks of 9-11, Colonel Mulholland commanded Joint Special Operations Task Force-North (Task Force Dagger) in the opening days of Operation ENDURING FREEDOM and, later, Combined Joint Special Operations Task Force-West (Task Force Dagger) in the initial campaign of Operation IRAQI FREEDOM.
LTG Mulholland’s (Ret) overseas assignments included two tours in the former Panama Canal Zone, command of the 1st Battalion, 1st Special Forces Group (ABN), Okinawa, Japan and as the Chief, Office of Military Cooperation, Kuwait. LTG Mulholland (Ret) served at and completed his final tour on active duty as the Associate Director of Military Affairs, Central Intelligence Agency. LTG Mulholland (Ret) is married to the former Miriam Mitchell. Together, they have 4 grown children and 5 grandchildren. LTG Mulholland (Ret) and Miriam now operate Mulholland Consulting, LLC in Alexandria, Virginia.

Tim Szymanski, VADM, U.S. Navy (Ret.)
Member, Veterans Advisory Council
Tim Szymanski, VADM, U.S. Navy (Ret.)
Member, Veterans Advisory Council
Tim has served in many Navy and Joint Special Operations assignments as a Navy Special Warfare Officer (SEAL) for over 36 years. He most recently served as the Deputy Commander for United States Special Operations Command (USSOCOM) after serving as the Commander of Naval Special Warfare (NSW). In both roles he oversaw the manning, equipping and training, and employment of NSW and joint special operations forces, of 11,000 and 73,000 uniformed and civilian personnel, respectively.
He has an extensive background in raising, equipping, and training Navy, allied and joint special operations forces and has served operationally in Iraq, Afghanistan, Haiti, and other places of crises. As Deputy Commander USSOCOM and as Commander NSW he spearheaded force design and development initiatives, led organizational culture reviews and implementation plans, and developed leaders throughout the force.
Keenly aware of the detrimental effects of invisible wounds on Force and Family Readiness, he established policies and developed lines of effort to monitor, protect and enhance warfighter brain health.
More from our VAC

- Blog
A Navy SEAL Talks Commitment and Care
- Blog
Reflections On The Impact Of 9/11 From A Secret Service Agent Who Was There – And Whose Family Was Forever Changed
- My Story
Bob Harward
- My Story
Frank Larkin
A Navy SEAL Talks Commitment and Care
Reflections On The Impact Of 9/11 From A Secret Service Agent Who Was There – And Whose Family Was Forever Changed
Bob Harward
Frank Larkin
More recently, Mr. Larkin served as the United States Senate Sergeant at Arms, and lead the Joint Improvised Explosive Device Defeat Organization (JIEDDO) within the Department of Defense. Having experienced the impact of military trauma both personally and professionally, Mr. Larkin is committed to improving veterans healthcare and will Chair our Veterans Advisory Council in 2019 to support the advancement of veterans brain health.