They are – but we aren’t. It’s time for that to change.
Nearly 350,000 service member and veterans have been diagnosed with traumatic brain injury (TBI) since 2001. Even more have post-traumatic stress disorder (PTSD). Twenty veterans commit suicide every day, most of them as a direct result of these conditions.
PTSD, TBI, and suicide represent an all-out epidemic.
In their urgent quests for relief, veterans are turning to alternative therapies ranging from yoga to swimming in shark tanks to bonding with parrots. The striking fact of these therapies, like many other more traditional treatments, is that they often have inconsistent results or aren’t reproducible. We simply know too little to systematically evaluate effective treatments for PTSD and TBI.
Since the approval of two antidepressants more than a decade ago, there have been no new medicines developed specifically to treat PTSD. We are doing what we can with these antidepressants, talk therapy, and alternative medicine, but it isn’t enough.A JAMA study published last year found that after treatment with the two leading forms of psychotherapy, 2 in 3 PTSD patients still met the criteria for the disorder.
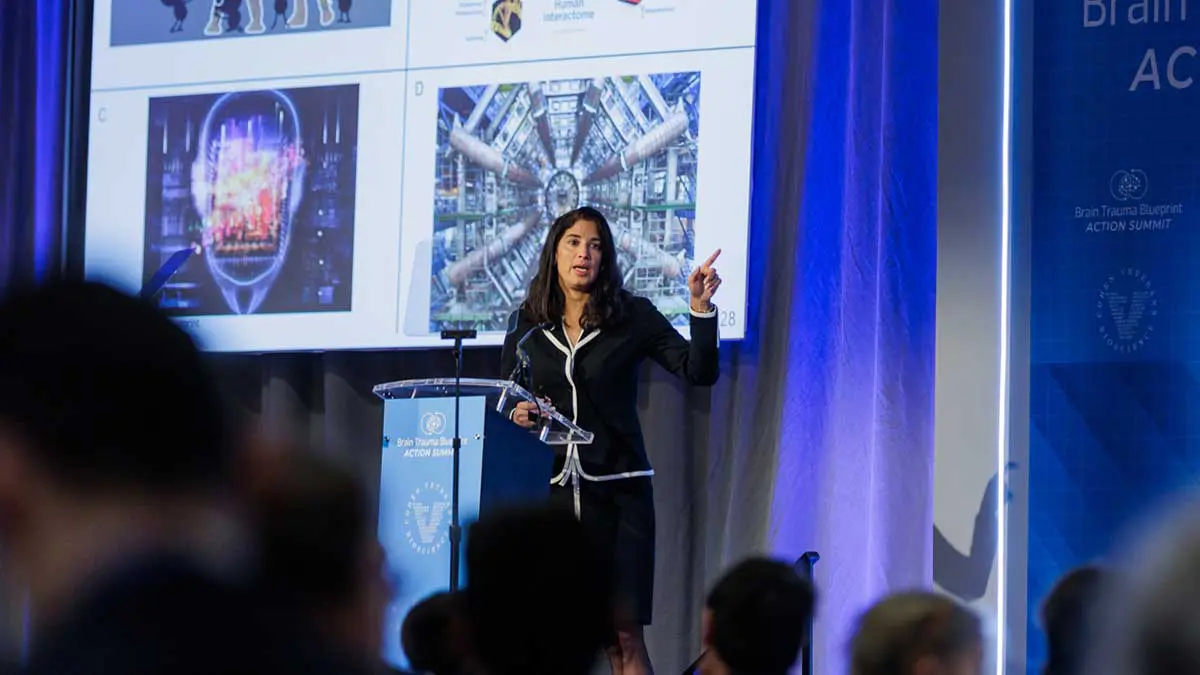
At a research summit last week in Washington, scientists, advocates, public officials, industry representatives, and others in the PTSD-TBI research community joined together to do better. It was sponsored by the organization that I lead, Cohen Veterans Bioscience, a nonprofit founded to drive transformational research into PTSD and TBI. The summit established a series of bold research goals and identified a range of obstacles that could block progress toward achieving them.
The goals are daring ones, worthy of the heroes and survivors whose lives are at stake. We believe that science can make it possible to effectively treat PTSD and the chronic effects of TBI effectively, as well as to understand their biology so precisely that we can predict who is likely to experience them and deliver personalized preventive therapy.
If the goals are ambitious, the obstacles are no less substantial. We currently have no mechanistic understanding of how PTSD, TBI, and related conditions arise. And there are no truly validated animal models in which to study these conditions.
The good news is that we have already made considerable scientific progress on PTSD and related conditions. Scientific papers on PTSD and TBI appeared last year at a rate of more than 10 a day. According to ClinicalTrials.gov, a registry of clinical trials run by the US National Library of Medicine, 117 trials are underway on PTSD and TBI and almost 400 more are currently recruiting participants.
This research has produced many promising leads. But they are not translating fast enough into diagnostic tools and treatments for service members and veterans. What is needed is a coordinated effort that brings together science and technology from the forefront of neuroscience, genetics, computer science, and medical imaging. Promising research from an array of fields must be scaled up and repeated to be sure that leads are worth pursuing into the costly and lengthy process of drug development.
My organization convened this week’s summit to stimulate and coordinate this process. We serve as a nonprofit research accelerator, bringing together the brightest minds and deploying the most innovative scientific tools. We aim to bring the science to scale while minimizing risk and maximizing efficiency and speed by allowing researchers to focus on science and ensure that their work produces meaningful returns for patients in the form of new knowledge, new tests, and new treatment.
That, ultimately, is the promise of science. Eureka moments may make headlines, but real success is difficult to achieve without directed, sustained, unglamorous effort. The science community bears an obligation to make that effort for the service members and veterans who protect us.
SEPTEMBER 26, 2016 – Published in STAT News
Magali Haas, MD, is CEO and president of Cohen Veterans Bioscience.