PTSD Facts
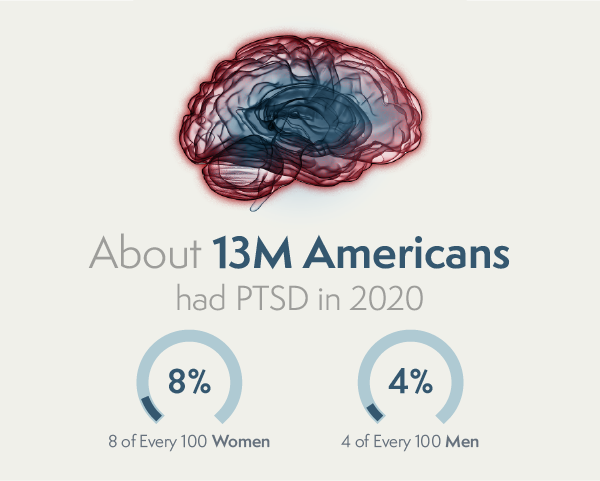
- In 2020, about 13 million Americans had PTSD. About 5 out of every 100 adults (or 5%) in the U.S. has PTSD in any given year.¹
- Women are more likely to develop PTSD than men. About 8 of every 100 women (or 8%) and 4 of every 100 men (or 4%) will have PTSD at some point in their life.¹
- Veterans are more likely to have PTSD than civilians. Veterans deployed to a war zone are also more likely to have PTSD than those who did not deploy.¹
What is Post-traumatic Stress Disorder (PTSD)?
Post-traumatic stress disorder (PTSD) can be complex and chronic and is a clinically diagnosed condition that occurs in individuals who experience or witness a traumatic event that involves the actual or possible threat of death, violence, or serious injury. Examples of traumatic events include experiencing or witnessing a natural disaster, serious accident, terrorist act, war/combat, rape, or being threatened with death, sexual violence, or serious injury. A traumatic event could also be learning about a close friend or family member experiencing a traumatic event. It can also be repeated exposure to the details of traumatic events, such as with first responders.
Following a traumatic event, most people will experience symptoms such as difficult memories, feeling on edge, or trouble sleeping. These short-term symptoms are known as acute stress disorder (ASD) and typically occur within the first month following the trauma. When the symptoms of ASD persist for longer than a month, an individual may have PTSD.
What is it like to live with Post-Traumatic Stress Disorder?
Read insights from Veterans and stories of people living with brain trauma.
Additional Resources on ‘What is Post-traumatic Stress Disorder (PTSD)?’
8.6M
8.6 million adults are diagnosed with PTSD in a given year in the United States.
10-20%
Approximately 10-20% (~ 300,000) Veterans who returned from the wars in Iraq and Afghanistan are suffering from PTSD.
2x
Women are twice as likely as men to develop PTSD.
More Likely

Symptoms of Post-traumatic Stress Disorder (PTSD)
Symptoms and signs of PTSD can vary in severity and fall into the following four types:
- Intrusive thoughts such as repeated, involuntary memories; distressing dreams; or flashbacks of the traumatic event.
- Avoidance of people, places, activities, objects, or situations that are reminders of the traumatic event or avoiding remembering, talking, or thinking about the traumatic event.
- Alterations in cognitions and mood, including being unable to remember important aspects of the traumatic event; negative thoughts and feelings about oneself or others (e.g., “I am bad,” “No one can be trusted”); feelings of anger, guilt or shame; a loss of interest in activities previously enjoyed; and feeling detached or estranged from others.
- Changes in arousal and reactivity, including being easily irritated, experiencing angry outbursts; behaving recklessly or in a self-destructive manner; being hypervigilant or easily startled; or having difficulties concentrating or sleeping.
Additional Resources on ‘Symptoms of Post-Traumatic Stress Disorder (PTSD)’
How is Post-traumatic Stress Disorder (PTSD) Diagnosed?
Additional Resources on ‘How is Post-traumatic Stress Disorder (PTSD) Diagnosed?’


Treatment for Post-traumatic Stress Disorder (PTSD)
PTSD is typically treated using psychotherapy or medications. Psychotherapy, or talk therapy, includes cognitive therapy, exposure therapy, and eye movement desensitization and reprocessing (EMDR). Medications such as antidepressants are often prescribed, and anti-anxiety medications may also be prescribed.
Although psychotherapy and medication can significantly reduce PTSD symptoms for some people, there is still great room for improvement. Only two drugs have been approved by the US Food and Drug Administration (FDA) to specifically treat PTSD. Both of these medications are in a class of drugs known as selective serotonin reuptake inhibitors (or SSRIs) and are also approved to treat depression. These medications do not reduce PTSD symptoms for everyone; only 20 – 30% of patients achieve remission (i.e., they no longer have PTSD). The nonresponse rate for psychotherapy is also high, with many people stopping early. As a result, treatment-resistant PTSD remains a significant problem.
We’re working to address this problem through robust and rigorous research to help better understand the biological underpinnings of PTSD. PTSD is a complex condition with different symptoms in different people. Gaining a better understanding of brain circuits and molecular pathways causing symptoms can enable better diagnoses and more effective treatments that target those circuits or pathways.
Additional Resources on ‘Treatment for Post-traumatic Stress Disorder (PTSD)’
Veterans and Post-traumatic Stress Disorder (PTSD)
For Veterans living with PTSD and brain injury, statistics show the invisible wounds continue long after they return home.
The invisible wounds of war—including post-traumatic stress (PTSD)—are common among those with military experience. Living with these conditions can be challenging for the person with the diagnosis, their family members, and their caregivers.
Additional Resources on ‘Veterans and Post-traumatic Stress Disorder (PTSD)’


Post-traumatic Stress Disorder (PTSD) and Suicide Risk
Veterans living with PTSD are at a higher risk of suicide, as they spend years waiting for a diagnosis that will explain their symptoms or cycle through numerous treatments without finding relief.
Brain trauma changes the structure and function of the brain and can lead to various cognitive, physical, and emotional symptoms. Some of these symptoms may appear immediately after the traumatic event or brain injury, while others may be delayed, emerging months, or even years later. This complexity makes diagnosing and treating PTSD more difficult.
Delayed diagnosis and ineffective treatments can result in the most devastating outcome of all, suicidality. For the first time in our nation’s history, suicides from invisible wounds are outpacing the number of in-theatre deaths from physical wounds.
We must treat the underlying conditions that increase the risk of suicide.
- Despite decades of promising research and billions spent on clinical studies, there are no cures for the invisible wounds.
- Patients are diagnosed based on subjective, patient-reported symptoms, not in an objective way based on their unique biology.
- We lack reliable, evidence-based treatments.
Additional Resources on ‘Post-traumatic Stress Disorder (PTSD) and Suicide Risk’
What is complex PTSD?
Complex PTSD (CPTSD) can arise following exposure to severe or prolonged traumatic stressors, often where a person is unable to escape the trauma (e.g., someone experiencing sexual abuse, childhood neglect, or human trafficking). While people suffering from CPTSD can experience symptoms of PTSD (e.g., intrusive thoughts, changes in reactivity, avoidance tendencies), they may also experience difficulties with interpersonal relationships, difficulties with impulse control, an inability to tolerate negative emotional states, and often have a negative concept of themselves.2, 3


PTSD in Women
Although women witness or experience fewer traumatic events in their lifetime in relation to men, women have an increased risk of experiencing PTSD in their lifetime. This may be partially attributable to higher rates of sexual assault and intimate partner violence among women. Biological factors may also explain why women experience an increased burden of PTSD symptoms and a longer course of illness compared to men.4
Sleep and PTSD
Sleep is key to maintaining brain health; research suggests the neural activity during sleep removes toxins from the brain that can build up during the day.5
Sleep disruptions are one of the most debilitating symptoms of PTSD, and are a risk factor for suicide. PTSD can affect sleep in a variety of ways, including insomnia, frequent or repetitive nightmares, and disruptive behaviors during the night.6
A patter of poor sleep can lead to:- Sluggish behavior and reaction times
- Difficulty with memory, learning, and concentration
- Irritable feelings and mood swings
- Suicidal ideation or thoughts about self-harm
Many treatments are effective at improving sleep disturbances in people with PTSD. Sleep disturbances are an important symptom to manage, and improving sleep can also improve quality of life for people living with PTSD.7

What is it like living with symptoms of PTSD?
Individuals dealing with PTSD symptoms are not alone. Here are stories from people living with PTSD.
-
 "On the outside, I probably seemed normal. But on the inside, I struggled to feel safe, I struggled to find hope, and I struggled to engage in life beyond going through the motions...I lost the ability to close my eyes without being transported back to my trauma. I stopped doing anything and everything, and often felt disoriented and overcome by panic. I went from being a straight A student in the honors program to dropping out of college. But still, I did not seek help, overcome by fear, shame and guilt."
"On the outside, I probably seemed normal. But on the inside, I struggled to feel safe, I struggled to find hope, and I struggled to engage in life beyond going through the motions...I lost the ability to close my eyes without being transported back to my trauma. I stopped doing anything and everything, and often felt disoriented and overcome by panic. I went from being a straight A student in the honors program to dropping out of college. But still, I did not seek help, overcome by fear, shame and guilt."
Read Chantelle's Story
-
 "I hope to be able to bring people hope by telling my story. By telling how I moved on. By telling about post-traumatic growth. I think getting mentally better requires a 360 degree view on everything. If your body is unfit, your mind probably is as well, and vice versa. That’s how I got better, I worked on all the small details. It all adds up. I’d like to share that view with others as well."
"I hope to be able to bring people hope by telling my story. By telling how I moved on. By telling about post-traumatic growth. I think getting mentally better requires a 360 degree view on everything. If your body is unfit, your mind probably is as well, and vice versa. That’s how I got better, I worked on all the small details. It all adds up. I’d like to share that view with others as well."
Watch Christian's Story
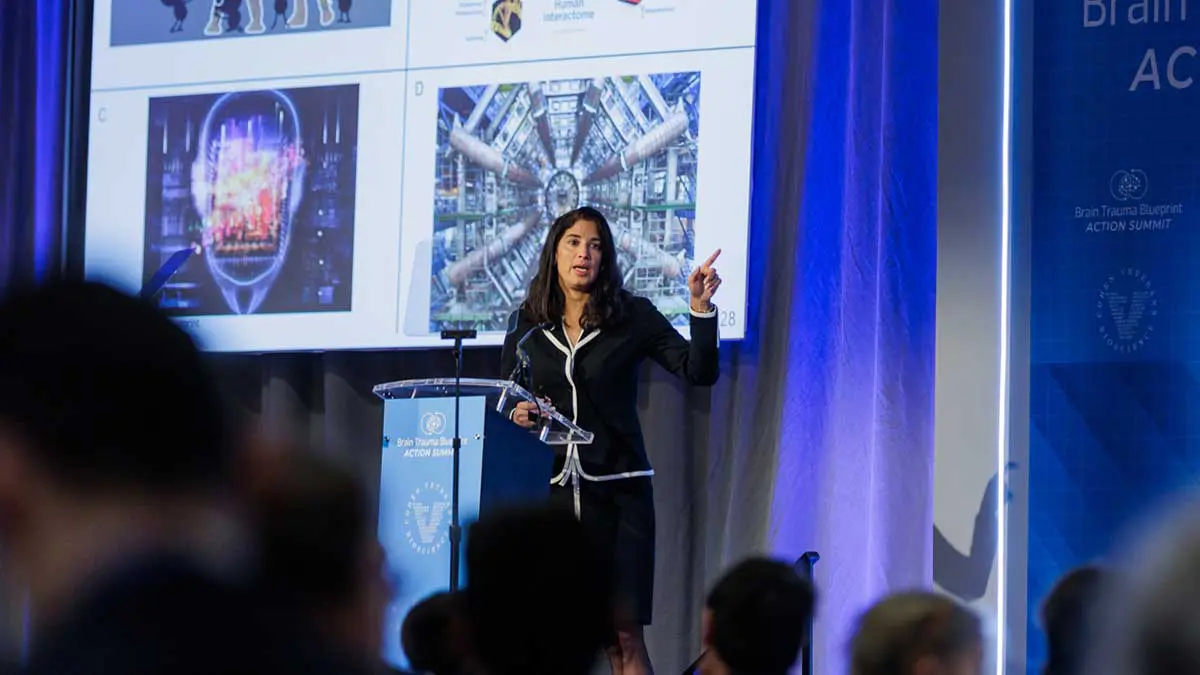
Our Post-traumatic Stress Disorder (PTSD) Research That is Making a Difference
Our mission is to fast-track and advance solutions to diagnose and treat PTSD. No one who experiences brain trauma should suffer the effects for a lifetime.
Learn how our research advances solutions for patients living with the effects of PTSD
Learn about our clinical studies related to PTSD
Additional Resources on ‘Post-traumatic Stress Disorder (PTSD) and Research’

Resources and Further Reading
- If you have taken steps to end your life, call 911 immediately.
- National Suicide Prevention Hotline – Dial 988
- National Sexual Assault Hotline – (800) 656-HOPE
- National Center for PTSD – Veterans Crisis Line – (800) 273-8255
- Women’s Veterans Call Center – (855) VA-Women
Sources / Citations
1 U.S. Department of Veterans Affairs, PTSD: National Center for PTSD
4 Post-traumatic stress disorder in women: epidemiological and treatment issues. CNS Drugs; 2005.
5 How Sleep Clears the Brain. NIH Research Matters; October 2013.
Cohen Veterans Bioscience (CVB) is a non-profit 501(c)(3) public charity research organization and does not offer medical advice. CVB encourages you to seek medical advice from a physician or healthcare provider if you have questions regarding a medical condition or to call 911 or go to the nearest hospital if you find that you or someone you are concerned about is in an emergency situation.